Previous issues
- Page Path
- HOME > Browse Articles > Previous issues
- Up-to-date treatment of acetaminophen poisoning
- Phil Chung Sung, Moon Jeongmi, Chun Byeongjo
- J Korean Soc Clin Toxicol. 2022;20(2):39-44. Published online December 31, 2022
- DOI: https://doi.org/10.22537/jksct.2022.20.2.39
- 295 View
- 37 Download
-
 Abstract
Abstract
 PDF
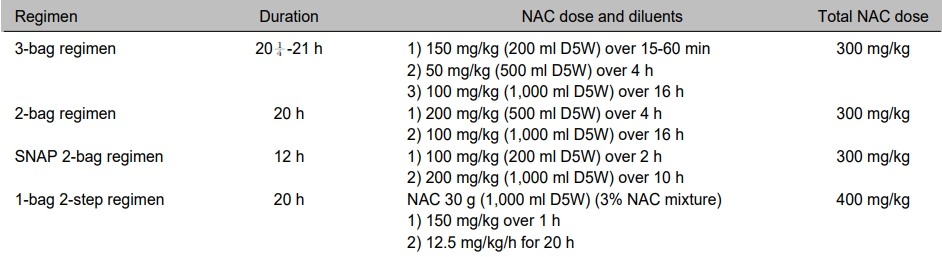
PDF - N-Acetylcysteine (NAC) is the standard antidote treatment for preventing hepatotoxicity caused by acetaminophen (AAP) poisoning. This review summarizes the recent evidence for the treatment of AAP poisoning. Several alternative intravenous regimens of NAC have been suggested to improve patient safety by reducing adverse drug reactions and medication errors. A two-bag NAC infusion regimen (200 mg/kg over 4 h, followed by 100 mg/kg over 16 h) is reported to have similar efficacy with significantly reduced adverse reactions compared to the traditional 3-bag regimen. Massive AAP poisoning due to high concentrations (more than 300-lines in the nomogram) needs to be managed with an increased maintenance dose of NAC. In addition to NAC, the combination therapy of hemodialysis and fomepizole is advocated for severe AAP poisoning cases. In the case of a patient presenting with an altered mental status, metabolic acidosis, elevated lactate, and an AAP concentration greater than 900 mg/L, hemodialysis is recommended even if NAC is used. Fomepizole decreases the generation of toxic metabolites by inhibiting CYP2E1 and may be considered an off-label use by experienced clinicians. Since the nomogram cannot be applied to sustained-release AAP formulations, all potentially toxic sustained-release AAP overdoses should receive a full course of NAC regimen. In case of ingesting less than the toxic dose, the AAP concentration is tested twice at an interval of 4 h or more; NAC should be administered if either value is above the 150-line of the nomogram.
- Epidemiology of patients with snake bite or envenomation in emergency department: NEDIS (National Emergency Department Information System)
- Lee Serok, Jeon Woochan
- J Korean Soc Clin Toxicol. 2022;20(2):45-50. Published online December 31, 2022
- DOI: https://doi.org/10.22537/jksct.2022.20.2.45
- 339 View
- 28 Download
-
 Abstract
Abstract
 PDF
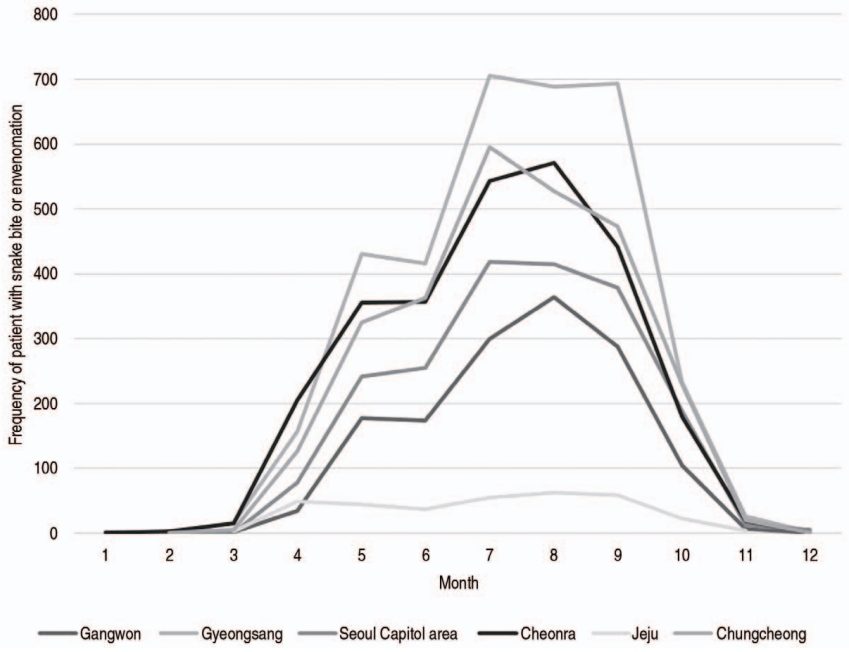
PDF - Purpose: This study utilizes the NEDIS (National Emergency Department Information System) database to suggest a predictive model for snakebite and envenomation in Korea by analyzing the geographical distribution and seasonal variation of snakebite patients visiting the ER. Methods: This was a retrospective study on snakebite patients visiting the ER using the NEDIS database from January 2014 to December 2019. The subjects include patients with the KCD (Korea Standard Classification of Disease) disease code T63.0 (Toxic effect of contact with snake venom). Geographical location, patient gender, patient age, date of ER visit, treatment during the ER stay, and disposition were recorded to analyze the geographical distribution and seasonal variation of snakebite patients in Korea. Results: A total of 12,521 patients were evaluated in this study (7,170 males, 54.9%; 5,351 females, 40.9%). The average age was 58.5±17.5 years. In all, 7,644 patients were admitted with an average admission time of 5.04±4.7 days, and 2 patients expired while admitted. The geographical distribution was Gyeongsang 3,370 (26.9%), Cheonra 2,692 (21.5%), Chungcheong 2,667 (21.3%), Seoul Capital area 1,999 (16.0%), Kangwon 1,457 (11.6%), and Jeju 336 (2.7%). The seasonal variation showed insignificant incidences in winter and higher severity in spring and summer than in fall: winter 27 (0.2%), spring 2,268 (18.1%), summer 6,847 (54.7%), and fall 3,380 (27.0%). Conclusion: Patients presenting with snakebites and envenomation in the emergency room were most common in the Gyeongsang area and during summer. The simple seasonal model predicted that 436 snakebites and 438 envenomation cases occurred in July and August. The results of this study can be applied to suitably distribute and stock antivenom. Appropriate policies can be formed to care for snakebite patients in Korea.
- Rhabdomyolysis induced by venomous snake bite
- Lee Jungho, Moon Jeongmi, Chun Byeongjo
- J Korean Soc Clin Toxicol. 2022;20(2):51-57. Published online December 31, 2022
- DOI: https://doi.org/10.22537/jksct.2022.20.2.51

- 173 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - Purpose: Despite previous studies reporting the development of rhabdomyolysis (RM), this affliction tends to be neglected as an envenomation sign in South Korea. The current retrospective study investigates the prevalence and prognosis of RM after a snakebite. We further searched for predictors of snakebite-induced RM, which can be observed at presentation. Methods: This study included 231 patients who presented to the ED within 24 hours after a snakebite. The patients were classified according to the severity of RM, and the data, comprising baseline characteristics and clinical course including the level of creatine kinase (CK), were collected and compared according to the severity of RM. Results: The prevalence of RM and severe RM were determined to be 39% and 18.5%, respectively. Compared to the group without RM or with mild RM, the group with severe RM had a higher grade of local swelling, a higher frequency of acute kidney injury and neurotoxicity, and a greater need for renal replacement therapy and vasopressor administration. However, the incidence of acute renal injury in the RM group was 7.7%, with two patients needing renal replacement therapy. No mortalities were reported at discharge. Results of the multinomial logistic regression model revealed that the WBC levels are significantly associated with the risk of severe RM. Conclusion: RM should be considered the primary clinical sign of snake envenomation in South Korea, although it does not seem to worsen the clinical course. In particular, physicians should pay attention to patients who present with leukocytosis after a snakebite, which indicates the risk of developing RM, regardless of the CK level at presentation.
- Clinical features related to alcohol co-ingestion of deliberate self-poisoning patients visiting the emergency department
- Won Kim Gyu, Jeong Lee Woon, Kim Daehee, Young Lee June, Yun Kim Sang, Jeong Sikyoung, Hong Sungyoup, Hee Woo Seon
- J Korean Soc Clin Toxicol. 2022;20(2):58-65. Published online December 31, 2022
- DOI: https://doi.org/10.22537/jksct.2022.20.2.58
- 184 View
- 12 Download
-
 Abstract
Abstract
 PDF
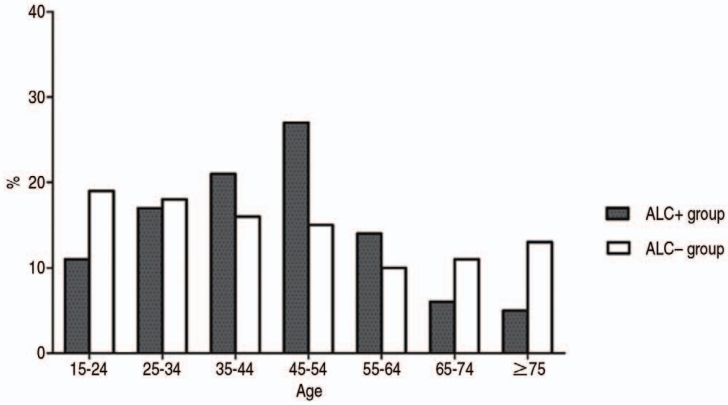
PDF - Purpose: Alcohol is one of the most commonly co-ingested agents in deliberate self-poisoning (DSP) cases presenting at the emergency department (ED). The increased impulsivity, aggressiveness, and disinhibition caused by alcohol ingestion may have different clinical features and outcomes in cases of DSP. This study investigates whether alcohol co-ingestion affects the clinical features and outcomes of DSP patients in the ED. Methods: This was a single-center retrospective study. We investigated DSP cases who visited our ED from January 2010 to December 2016. Patients were classified into two groups: with (ALC+) or without (ALC–) alcohol co-ingestion. The clinical features of DSP were compared by considering the co-ingestion of alcohol, and the factors related to discharge against medical advice (AMA) of DSP were analyzed. Results: A total of 689 patients were included in the study, with 272 (39.5%) in the ALC+ group. Majority of the ALC+ group patients were middle-aged males (45-54 years old) and arrived at the ED at night. The rate of discharge AMA from ED was significantly higher in the ALC+ group (130; 47.8%) compared to the ALC– group (p=0.001). No significant differences were obtained in the poisoning severity scores between the two groups (p=0.223). Multivariate analysis revealed that alcohol co-ingestion (odds ratio [OR]=1.42; 95% confidence interval [CI], 1.01-1.98), alert mental status (OR=1.65; 95% CI, 1.17-2.32), past psychiatric history (OR=0.04; 95% CI, 0.01-0.28), age >65 years (OR=0.42; 95% CI, 0.23-0.78), and time from event to ED arrival >6 hrs (OR=0.57; 95% CI, 0.37-0.88) were independent predictive factors of discharge AMA (p=0.043, p=0.004, p=0.001, p=0.006, and p=0.010, respectively). Conclusion: Our results determined a high association between alcohol co-ingestion and the outcome of discharge AMA in DSP patients. Emergency physicians should, therefore, be aware that DSP patients who have co-ingested alcohol may be uncooperative and at high risk of discharge AMA.
- Characteristics of poisoning patients visiting emergency departments before and after the COVID-19 pandemic
- Jae Kee Seung, Cho Yongil, Kang Hyunggoo, Ho Lim Tae, Oh Jaehoon, Sung Ko Byuk, Lee Juncheol
- J Korean Soc Clin Toxicol. 2022;20(2):66-74. Published online December 31, 2022
- DOI: https://doi.org/10.22537/jksct.2022.20.2.66

- 799 View
- 16 Download
- 2 Citations
-
 Abstract
Abstract
 PDF
PDF - Purpose: This study investigates the characteristics and prognosis of acute poisoning patients visiting nationwide emergency departments before and after the Coronavirus disease 2019 (COVID-19) pandemic. Data were obtained from the National Emergency Department Information System (NEDIS). Methods: This nationwide retrospective observational study included acute poisoning patients who visited the emergency departments between February 1 to December 31, 2020, which has been determined as the pandemic period. The same periods in 2018 and 2019 were designated as the control periods. The primary outcome assessed was the length of stay in emergency departments (EDLOS). The secondary outcomes examined were intensive care unit admission rate and in-hospital mortality rate before and after the pandemic. A subgroup analysis was performed for inpatients and intentional poisoning patients. Results: A total of 163,560 patients were included in the study. During the pandemic, the proportion of women increased from 50.0% in 2018 and 50.3% in 2019 to 52.5% in 2020. Patients aged 20-29 years increased from 13.4% in 2018 and 13.9% in 2019 to 16.6% in 2020. A rise in cases of intentional poisoning was also noted - from 33.9% in 2018 and 34.0% in 2019 to 38.4% in 2020. Evaluating the hospitalized poisoned patients revealed that the EDLOS increased from 3.8 hours in 2018 and 3.7 hours in 2019 to 4.2 hours in 2020. ICU admissions were also markedly increased (2018, 48.2%; 2019, 51.8%; 2020, 53.2%) among hospitalized patients. Conclusion: The COVID-19 pandemic has changed the epidemiology, clinical characteristics, and prognosis of acute poisoning patients visiting nationwide emergency departments in Korea. The proportion of young adults, women, and intentional poisoning patients has increased after the COVID-19 pandemic. Prolonged length of stay at the emergency department and an increased rate of intensive care unit admissions were determined in hospitalized acute poisoning patients.
-
Citations
Citations to this article as recorded by- Demographic characteristics of patients admitted to the emergency department for intoxication and a time series analysis during the COVID-19 period
Bongmin Son, Nayoon Kang, Eunah Han, Gina Yu, Junho Cho, Jaiwoog Ko, Taeyoung Kong, Sung Phil Chung, Minhong Choa
Journal of The Korean Society of Clinical Toxicology.2023; 21(2): 92. CrossRef - Changes in the characteristics of acute carbon monoxide poisoning patients who visited the emergency department during the COVID-19 pandemic
Jun bo Sim, Tae kyu Ahn, Hyun Kim
Journal of The Korean Society of Clinical Toxicology.2023; 21(2): 108. CrossRef
- Demographic characteristics of patients admitted to the emergency department for intoxication and a time series analysis during the COVID-19 period
- Prediction of pathogen positive-culture results in acute poisoning patients with suspected aspiration
- Sungha Baek, Sungwook Park
- J Korean Soc Clin Toxicol. 2022;20(2):75-81. Published online December 31, 2022
- DOI: https://doi.org/10.22537/jksct.2022.20.2.75
- 145 View
- 5 Download
-
 Abstract
Abstract
 PDF
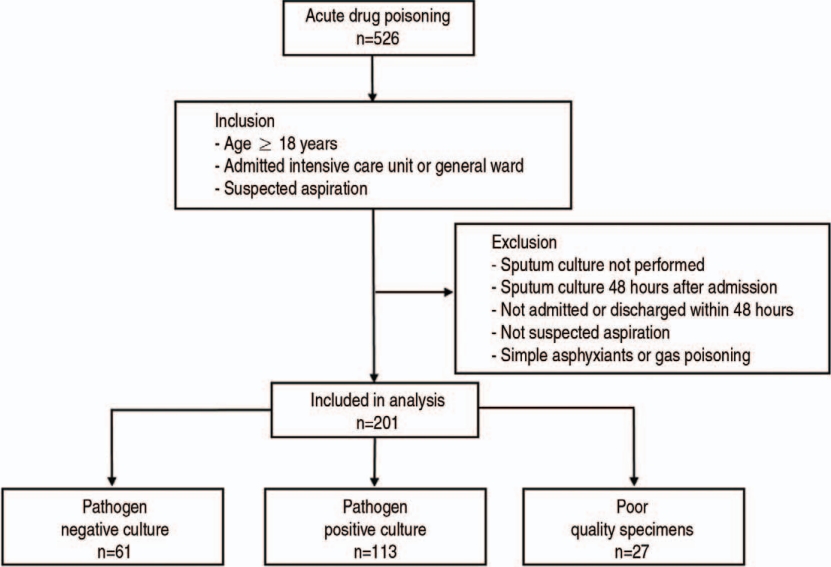
PDF - Purpose: This study sought to compare the characteristics of patients with pathogen-positive and negative cultures, and to investigate factors predicting pathogen-positive culture results in patients of acute poisoning with suspected aspiration. Methods: Consecutive patients with acute poisoning admitted to an intensive care unit between January 2016 and December 2018 were retrospectively studied. Respiratory specimens were collected from the enrolled patients at the time of the suspected aspiration. We compared the characteristics of patients with pathogen-positive and negative culture results and analyzed the causative pathogens. Results: Among the 526 patients, 325 showed no clinical features that could be attributed to aspiration, and 201 patients had clinical features suggestive of aspiration. Of these, 113 patients had pathogen-positive culture, 61 were negative, and the specimens of 27 patients contained poor-quality sputum. In univariate analysis, patients with a positive culture showed a longer time to culture from ingestion (p=0.01), faster heart rate (p=0.01), and higher partial pressure of arterial oxygen to the fraction of inspired oxygen (PaO2/FiO2) (p=0.02) than patients with negative culture. Multivariate analysis demonstrated that PaO2/FiO2 (adjusted odd ratio, 1.005; 95% confidence interval [CI], 1.002-1.008; p=0.005) was a significant risk factor for pathogen-positive culture. The area under the receiver operating characteristic curve of PaO2/FiO2 was 0.591 (95% CI, 0.510-0.669, p=0.05). Gram-negative pathogens (GNPs) were predominant and at least one GNP was observed in 84 (73.3%) patients among those with pathogen positive culture. Conclusion: We failed to find any clinical factors associated with positive culture results. Antibiotics that cover GNPs could be considered when deciding the initial antibiotic regimen at the time of suspected aspiration.
- Cardiac arrest and severe encephalopathy following e-cigarette nicotine intoxication: a case report
- Park Jinwon, Yun Sunghyun
- J Korean Soc Clin Toxicol. 2022;20(2):82-85. Published online December 31, 2022
- DOI: https://doi.org/10.22537/jksct.2022.20.2.82

- 211 View
- 10 Download
-
 Abstract
Abstract
 PDF
PDF - Traditionally, most cases of nicotine poisoning have been due to ingestion of nicotine pesticides. However, the increasing use of electronic cigarettes (e-cigarettes) has resulted in both intentional and unintentional exposure to concentrated liquid nicotine or “eliquid” leading to an increase in nicotine poisoning cases. However, fatalities following the ingestion of the e-liquid are extremely rare. We report a rare case of cardiac arrest and severe encephalopathy following the intentional ingestion of e-liquid. We present the case of a 20-year-old woman who intentionally ingested liquid nicotine intended for e-cigarette use. She was found in asystole and experienced a return of spontaneous circulation (ROSC) after undergoing approximately 46 mins of cardiopulmonary resuscitation. Her plasma nicotine levels were >500 ng/ml. Despite aggressive supportive care, she was found to have encephalopathy consistent with severe anoxic brain injury on magnetic resonance imaging. In recent times, there have been some reports of deaths following liquid nicotine ingestion. Our case illustrates the potential for fatal nicotine toxicity from ingestion of e-cigarettes.

 KSCT
KSCT



 First
First Prev
Prev



 Korean Society of Clinical Toxicology
Korean Society of Clinical Toxicology